Page 46 - รายงานประจำปี ๒๕๕๕ ศูนย์องค์รวมเพื่อการศึกษาและบำบัดโรคมะเร็ง คณะแพทยศาสตร์
P. 46
รายงานประจ�าปี 2555
ศูนย์องค์รวมเพื่อการศึกษาและบ�าบัดโรคมะเร็ง
INCREASE OF PATIENTS’ MEDICATION KNOWLEDGE BY
MEDICATION RECONCILIATION WITH INTENSIVE COUNSELING
Atittaya Yeela , Apinya Prisutkul , Maliwan Sukuntapan , Nannapat Pruphetkaew , Patrapim Sunpaweravong 1
1
1
2
1
1 Holistic Center for Cancer Study and Care (HOCC-PSU), Division of Medical Oncology,
2 Division of Epidemiology, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand;
Introduction : Patients with cancer may have chemotherapy and other medications to palliate
symptoms or co-morbidities. Medication reconciliation, comparing pre-existing medication to the
current one, is a notable step to improve quality of care. Moreover, adding intensive counseling may
increase efficiency of anticancer and co-morbidities therapy.
Materials and method : This research aimed primarily to compare medical knowledge pre- and
post- medication reconciliation with or without intensive counseling. Other objectives were to determine
incidence and severity of medication error, response, and survival of patients.
Result : One hundred and twenty-two patients gave their consent and completed the study process.
Sixty-two patients were assigned to the intervention group and sixty patients to the control. In the control,
no differences of pre- and post- test medication knowledge scores were observed. In the intervention,
mean medication knowledge scores of the post-test were significantly higher than the pre-test (shown
in table 1). Medication error events regarding dose omission and improper dose, however, were equal
to 50% in the control group whereas 33.33% and 66.67%, respectively, in the intervention group.
Differential blood pressure in same patients between visit 1 and visit 2 (control vs intervention group)
were shown in Table 2. A tendency of overall survival improvement were shown in figure 1. Effects on
response of anticancer were shown in figure 2.
Conclusion : Medication reconciliation with intensive counseling to outpatient oncologic patients
improved their medication knowledge significantly and revealed a promising tendency of overall
survival improvement. This intervention should be considered to be implemented into a standard
oncology care to improve the treatment outcome and encourage patient safety environment.
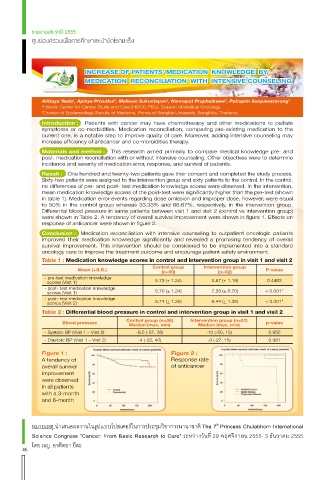
Table 1 : Medication knowledge scores in control and intervention group in visit 1 and visit 2
Control group Intervention group
Mean (+S.D.) (n=60) (n=62) P-value
- pre-test medication knowledge
scores (Visit 1) 5.73 (+ 1.24) 5.87 (+ 1.19) 0.4482
- post- test medication knowledge
scores (Visit 1) 5.70 (+ 1.24) 7.28 (+ 0.70) < 0.001*
- post- test medication knowledge
scores (Visit 2) 5.71 (+ 1.25) 6.44 (+ 1.35) < 0.001*
Table 2 : Differential blood pressure in control and intervention group in visit 1 and visit 2
Control group (n=36) Intervention group (n=31)
Blood pressure p-value
Median (max, min) Median (max, min)
- Systolic BP (Visit 1 – Visit 2) -8.5 (-57, 36) -10 (-50, 15) 0.955
- Diastolic BP (Visit 1 – Visit 2) -4 (-22, 40) -3 (-27, 15) 0.981
Figure 1 : Figure 2 :
A tendency of Response rate
overall survival of anticancer
improvement
were observed
in all patients
with a 3-month
and 6-month
หมายเหตุ น�าเสนอผลงานในรูปแบบโปสเตอร์ในการประชุมวิชาการนานาชาติ The 7 Princess Chulabhorn International
th
Science Congress “Cancer: From Basic Research to Cure” ระหว่างวันที่ 29 พฤศจิกายน 2555- 3 ธันวาคม 2555
โดย ภญ. อาทิตยา ยีละ
46